Free Annual Physical Examination Form
Form Preview Example
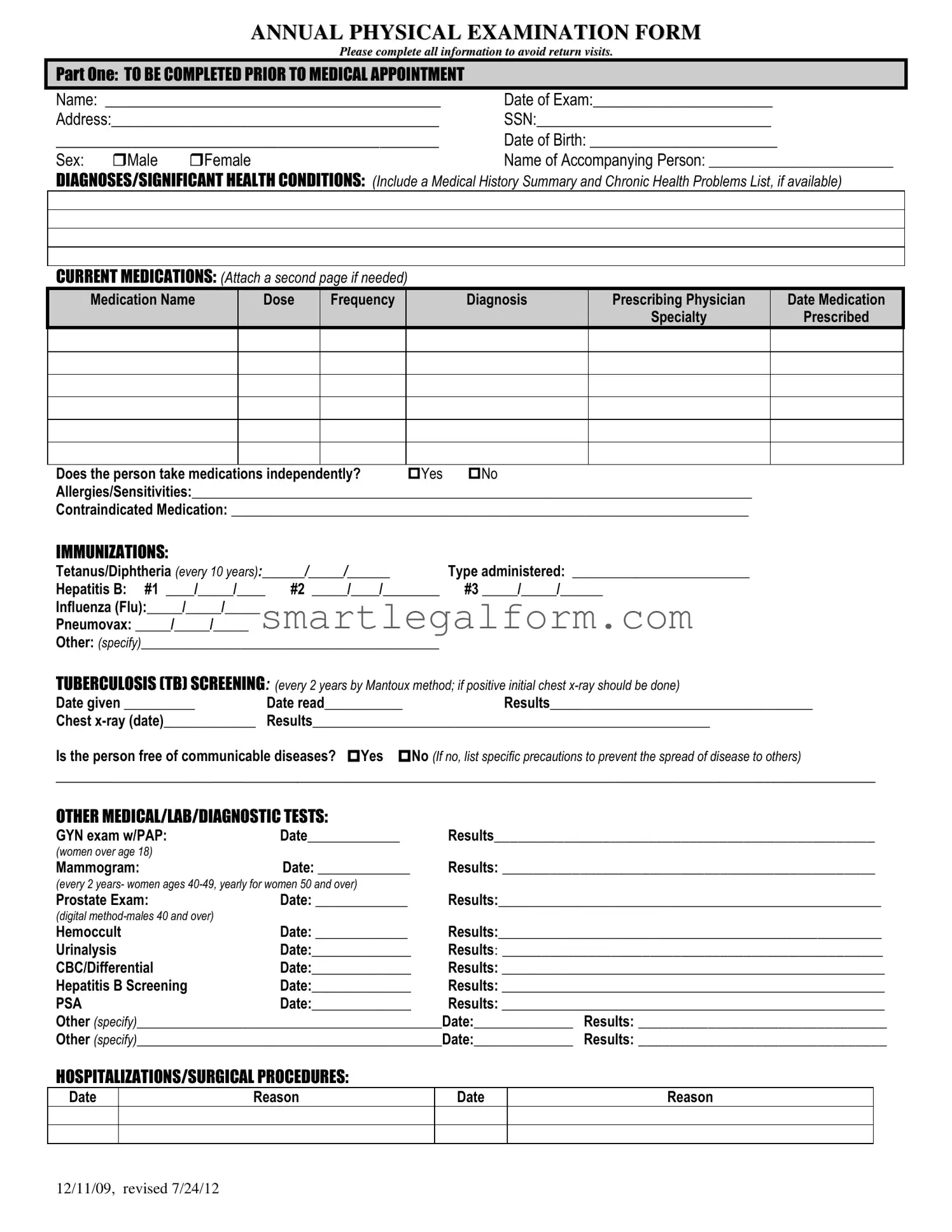
ANNUAL PHYSICAL EXAMINATION FORM
Please complete all information to avoid return visits.
PART ONE: TO BE COMPLETED PRIOR TO MEDICAL APPOINTMENT
Name: ___________________________________________ |
Date of Exam:_______________________ |
Address:__________________________________________ |
SSN:______________________________ |
_____________________________________________ |
Date of Birth: ________________________ |
||
Sex: |
Male |
Female |
Name of Accompanying Person: __________________________ |
DIAGNOSES/SIGNIFICANT HEALTH CONDITIONS: (Include a Medical History Summary and Chronic Health Problems List, if available)
CURRENT MEDICATIONS: (Attach a second page if needed)
Medication Name |
Dose |
Frequency |
Diagnosis |
Prescribing Physician |
Date Medication |
|
|
|
|
Specialty |
Prescribed |
Does the person take medications independently? |
Yes |
No |
Allergies/Sensitivities:_______________________________________________________________________________ |
||
Contraindicated Medication: _________________________________________________________________________
IMMUNIZATIONS:
Tetanus/Diphtheria (every 10 years):______/_____/______ |
Type administered: _________________________ |
|
Hepatitis B: #1 ____/_____/____ |
#2 _____/____/________ |
#3 _____/_____/______ |
Influenza (Flu):_____/_____/_____ |
|
|
Pneumovax: _____/_____/_____ |
|
|
Other: (specify)__________________________________________ |
|
|
TUBERCULOSIS (TB) SCREENING: (every 2 years by Mantoux method; if positive initial chest |
||
Date given __________ |
Date read___________ |
Results_____________________________________ |
Chest |
Results________________________________________________________ |
|
Is the person free of communicable diseases? Yes No (If no, list specific precautions to prevent the spread of disease to others)
_________________________________________________________________________________________________________
OTHER MEDICAL/LAB/DIAGNOSTIC TESTS:
GYN exam w/PAP: |
Date_____________ |
Results_________________________________________________ |
(women over age 18) |
|
|
Mammogram: |
Date: _____________ |
Results: ________________________________________________ |
(every 2 years- women ages
Prostate Exam: |
Date: _____________ |
Results:______________________________________________________ |
|
(digital |
|
|
|
Hemoccult |
Date: _____________ |
Results:______________________________________________________ |
|
Urinalysis |
Date:______________ |
Results: _________________________________________________ |
|
CBC/Differential |
Date:______________ |
Results: ______________________________________________________ |
|
Hepatitis B Screening |
Date:______________ |
Results: ______________________________________________________ |
|
PSA |
Date:______________ |
Results: ______________________________________________________ |
|
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
HOSPITALIZATIONS/SURGICAL PROCEDURES:
Date
Reason
Date
Reason
12/11/09, revised 7/24/12

PART TWO: GENERAL PHYSICAL EXAMINATION
|
|
|
|
|
Please complete all information to avoid return visits. |
|
|
|
|
|
Blood Pressure:______ /_______ Pulse:_________ |
Respirations:_________ Temp:_________ Height:_________ |
Weight:_________ |
||||
|
|
EVALUATION OF SYSTEMS |
|
|
|
|
||
|
|
|
|
|
|
|
||
|
|
System Name |
|
Normal Findings? |
Comments/Description |
|
||
|
|
Eyes |
|
Yes |
No |
|
|
|
|
|
Ears |
|
Yes |
No |
|
|
|
|
|
Nose |
|
Yes |
No |
|
|
|
|
|
Mouth/Throat |
|
Yes |
No |
|
|
|
|
|
Head/Face/Neck |
|
Yes |
No |
|
|
|
|
|
Breasts |
|
Yes |
No |
|
|
|
|
|
Lungs |
|
Yes |
No |
|
|
|
|
|
Cardiovascular |
|
Yes |
No |
|
|
|
|
|
Extremities |
|
Yes |
No |
|
|
|
|
|
Abdomen |
|
Yes |
No |
|
|
|
|
|
Gastrointestinal |
|
Yes |
No |
|
|
|
|
|
Musculoskeletal |
|
Yes |
No |
|
|
|
|
|
Integumentary |
|
Yes |
No |
|
|
|
|
|
Renal/Urinary |
|
Yes |
No |
|
|
|
|
|
Reproductive |
|
Yes |
No |
|
|
|
|
|
Lymphatic |
|
Yes |
No |
|
|
|
|
|
Endocrine |
|
Yes |
No |
|
|
|
|
|
Nervous System |
|
Yes |
No |
|
|
|
|
|
VISION SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
HEARING SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
ADDITIONAL COMMENTS: |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
Medical history summary reviewed? |
Yes |
No |
|
|
||
Medication added, changed, or deleted: (from this appointment)__________________________________________________________
Special medication considerations or side effects: ________________________________________________________________
Recommendations for health maintenance: (include need for lab work at regular intervals, treatments, therapies, exercise, hygiene, weight control, etc.)
___________________________________________________________________________________________________________
Recommendations for manual breast exam or manual testicular exam: (include who will perform and frequency)____________________
___________________________________________________________________________________________________________
Recommended diet and special instructions: ____________________________________________________________________
Information pertinent to diagnosis and treatment in case of emergency:
___________________________________________________________________________________________________________
Limitations or restrictions for activities (including work day, lifting, standing, and bending): No Yes (specify)
___________________________________________________________________________________________________________ |
|||
Does this person use adaptive equipment? |
No |
Yes (specify):________________________________________________ |
|
Change in health status from previous year? No |
Yes (specify):_________________________________________________ |
||
This individual is recommended for ICF/ID level of care? (see attached explanation) Yes |
No |
||
Specialty consults recommended? No |
Yes (specify):_________________________________________________________ |
||
Seizure Disorder present? No Yes (specify type):__________________________________ Date of Last Seizure: ______________ |
|||
________________________________ |
_______________________________ |
_________________ |
|
Name of Physician (please print) |
Physician’s Signature |
|
Date |
Physician Address: _____________________________________________ |
Physician Phone Number: ____________________________ |
||
12/11/09, revised 7/24/12
Common mistakes
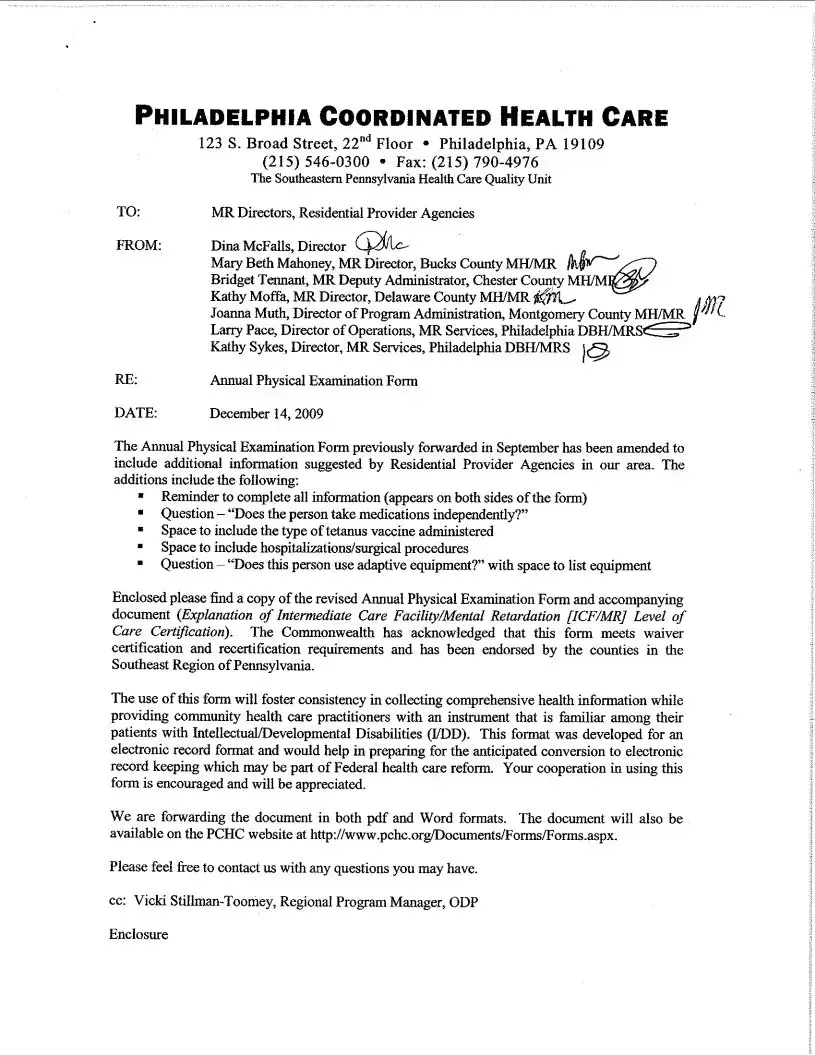
Completing the Annual Physical Examination form accurately is essential for ensuring a smooth medical appointment. However, many people make common mistakes that can lead to unnecessary delays or complications. Here are eight mistakes to watch out for.
First, failing to provide complete personal information is a frequent error. Many individuals skip filling in their full name, address, or date of birth. This information is crucial for identification and record-keeping. Double-checking these details before submitting the form can prevent a lot of hassle.
Another mistake is neglecting to list current medications. Some people forget to include over-the-counter drugs or supplements. It's important to provide a comprehensive list, including dosage and frequency. This information helps healthcare providers make informed decisions about your care.
Additionally, people often overlook allergies and sensitivities. Not mentioning these can lead to serious health risks during examinations or treatments. Make sure to detail any known allergies, including food, medication, and environmental factors.
In the immunizations section, many individuals fail to provide accurate dates or forget to mention previous vaccinations. Keeping a record of immunizations is essential for proper medical care. If unsure about your immunization history, consult your healthcare provider before filling out the form.
Another common error involves the evaluation of systems. Some individuals check "Yes" or "No" without providing comments or descriptions. This lack of detail can leave healthcare providers without crucial information about your health status. Clear communication in this section is vital for effective diagnosis and treatment.
People also frequently ignore the section about hospitalizations or surgical procedures. Omitting this information can result in incomplete medical histories. If you have undergone any procedures, list them with dates and reasons to ensure your healthcare provider has a full understanding of your medical background.
Moreover, failing to indicate whether a change in health status has occurred since the last examination is a mistake many make. This information can significantly impact your care plan. Be honest and thorough when answering this question.
Finally, some individuals forget to sign and date the form. This step is crucial for validating the information provided. Without a signature, the form may be considered incomplete, leading to delays in receiving care.
By being aware of these common mistakes and taking the time to fill out the Annual Physical Examination form carefully, individuals can ensure a more efficient and effective healthcare experience.
Dos and Don'ts
Completing the Annual Physical Examination form accurately is crucial for ensuring a smooth medical appointment. Here are some important dos and don'ts to keep in mind:
- Do fill out all sections completely to avoid delays.
- Do provide accurate personal information, including your name and date of birth.
- Do list all current medications, including dosage and frequency.
- Do mention any allergies or sensitivities clearly.
- Do indicate if you have had any recent hospitalizations or surgeries.
- Don't leave any required fields blank; incomplete forms may lead to return visits.
- Don't forget to check the box for communicable diseases if applicable.
- Don't omit details about your medical history or significant health conditions.
- Don't hesitate to ask for help if you are unsure about how to fill out any section.
By following these guidelines, you can help ensure that your Annual Physical Examination form is completed correctly and efficiently.
Other PDF Documents
CBP Form 6059B - Correct information from the form helps streamline the customs clearance process.
The Employment Verification Form is a document used by employers to confirm an individual's employment history, including job title, duration of employment, and sometimes salary information. This form plays a crucial role in the hiring process, as it helps potential employers assess a candidate's qualifications and reliability. For those looking for a resource to utilize, you can find the form at https://documentonline.org/blank-employment-verification-form/. Understanding how to properly fill out and submit this form can significantly impact both job seekers and employers alike.
Shower Sheets for Cna - The visual assessment is essential for proactive health management.
Similar forms
The Annual Physical Examination form is an essential document for assessing an individual's health status. Several other documents share similarities with this form, as they all aim to collect important health information. Here’s a look at seven such documents:
- Patient Intake Form: Like the Annual Physical Examination form, this document gathers personal details, medical history, and current medications from patients before their first visit to a healthcare provider.
- Medical History Questionnaire: This form focuses on a patient's past health issues, surgeries, and family medical history, similar to the section on diagnoses and significant health conditions in the Annual Physical Examination form.
- Medication Reconciliation Form: Both documents require patients to list their current medications, including dosages and prescribing physicians, ensuring that healthcare providers have accurate medication information.
- Immunization Record: Just as the Annual Physical Examination form tracks immunizations, this record documents vaccinations a patient has received, helping to maintain an up-to-date health profile.
- Referral Form: This document is used when a healthcare provider refers a patient to a specialist. It often includes pertinent medical history and current health concerns, mirroring the comprehensive evaluation found in the Annual Physical Examination form.
- Hold Harmless Agreement: A TopTemplates.info provides a thorough template for a Hold Harmless Agreement, which is essential for shifting liability in various situations, ensuring parties are protected from potential risks associated with their activities.
- Consent for Treatment Form: Similar to the Annual Physical Examination form, this document collects patient information and requires signatures, ensuring that patients understand and agree to the proposed medical evaluations and treatments.
- Follow-Up Visit Form: After an initial examination, this form is used to track changes in a patient’s health status and any new medications or treatments, much like the recommendations and changes noted in the Annual Physical Examination form.
These documents, while serving different purposes, all contribute to a comprehensive understanding of a patient's health and ensure that healthcare providers can deliver the best possible care.